
A Brief Suture History
1.30,000 BC Neolithic eyed needles
2.3,500 BC Edwin Smith Papyrus
3.210 AD Galen sewed gladiators w/gut
4.1887 sterile sutures introduced
5.1920 Merson invents the Swage

CLASSIFICATION OF SUTURES
●Absorbable vs. Permanent
Natural vs. Synthetic
Tensile strength loss over time
●Braided vs. Monofilament
BRAIDED VS MONOFILAMENT SUTURE
BRAIDED
●Handling better
●Knots more secure
●Softer
●No snitching, Clinching
●Infection risk hi, 10,000X less bact innoculum
●Freq spitting
MONOFILAMENT
●Lower infection risk
●Snitches easily
●Stiffer
●Less spitting
ABSORBABLE VS NON ABSORBABLE
ABSORBABLE
●No retained foreign body
●No late suture reaction
●Risk of premature tensile strength failure
●Elicits cellular response, ie wbc
NON-ABSORBABLE
●Permanent strength
●Useful anatomic marker
●Min inflamm response, monofil., relatively inert
●Long term FB effects, esp braided sutures
●Poor handling may cause loss of strength, eg instrument grasping, over stretch etc.


Absorbable suture strength loss
1.Vicryl and Vicryl rapide, coated (polyglactin)
a.3 wks
2.Monocryl (poliglecaprone)
a.2 wks
3.PDS (polydioanone)
a.4 wks
4.Gut; fast and chromic (collagen)
a. 1 wk
Natural material: Enzymatic Absorption w/ WBC response
Synthetic material: Hydrolysis with less WBC response
TYPES of ABSORBABLE SUTURE
MONOFILAMENT
●Monocryl (plus)
●PDS (plus)
●Gut
○Plain, fast, chromic
●Dyed vs Undyed
●Barbed (Stratafix)
BRAIDED
●Vicryl
●Vicryl rapide
●Dyed vs undyed
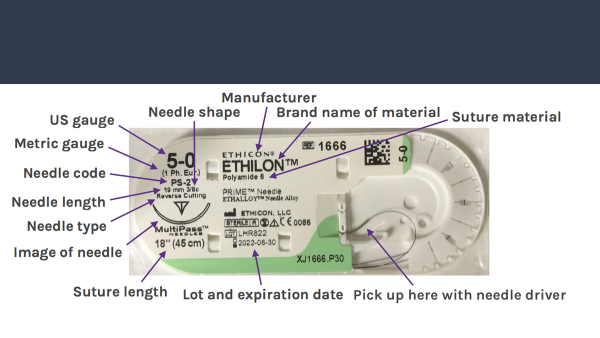
TYPES of NONABSORBABLE SUTURE
MONOFILAMENT
●Ethilon (nylon)
●Prolene (polypropylene)
●Pronova (blue)
●Steel
BRAIDED
●Nurolon (nylon)
●Mersilene (polyethylene)
●Ethibond (polyprop. green)
●Silk


TAPER
●Useful for vessels, delicate tissues, prone to propagating a tear
●Dull easily
CUTTING
●Many cutting tips
●Needle creates a small laceration in tissue
●Spatulated, Straight

WHAT SUTURE TO USE
SKIN of SCALP
●3–0 Prolene simple or vert.mattress as needed to evert
●Staples
●3–0 Monocryl Subcuticular
●Prineo System and Dermabond rare cases
SUBCUTANEOUS FAT LAYER and GALEA
●3–0 Monocryl buried in adipose
●2–0 Monocryl in Galea
●6–0 Prolene in face (forehead, brow, preauricular)
SOME TISSUE HANDLING TIPS
●Envision surgical tissue handling on a histologic level.
●Avoid crushing tissue, avoid excess or prolonged stretch
●Respect the cutaneous blood supply, cauterize judiciously
●Radiated tissue is anoxic on a cellular level due to obliterative arteritis, thus radiation injury worsens over time. Surgeon Beware!
●Place sutures evenly, without xs tension
●Minimize FB present in wound and hardware profile on overlying skin flap
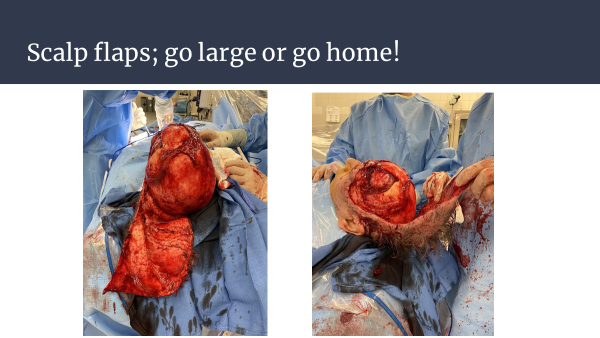
SOME (extracranial) SURGICAL TECHNIQUE TIPS
●Recognize and use old scars if possible, no signif. blood supply across the old scar. Keep Nitrobid close by…
●Err on side of larger flap design, not smaller.
●Protect scalp flap in long cases, keep moist, avoid excess tension in retraction, allow 5 min restoration of blood flow if flap is ischemic for >6 hrs.
●Undermine scalp at subperiosteal level to recruit laxity if needed. OK to undermine forehead to sup orbit and nasal root, cheek to zygoma, and occiput to nape of neck if SO, ST, Occip vessels are preserved.
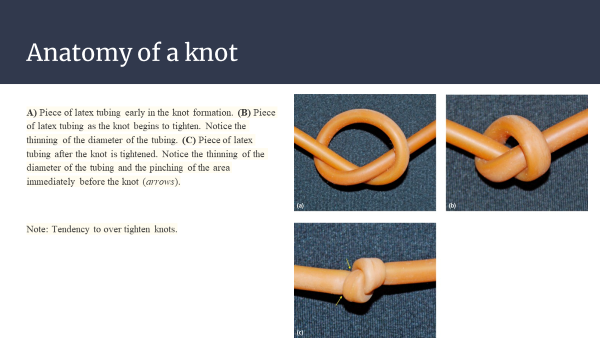
Suture Technique

WHEN TO REMOVE SUTURES
Suture scars result from epithelialization of suture tract, ie sutures in too long, or strangulation of tissue within suture loop, suture pulled too tight or excess po swelling.
SUTURE REMOVAL SCHEDULE
●Face; 5 days
●Scalp; 14 days
●Radiated scalp; 28 days



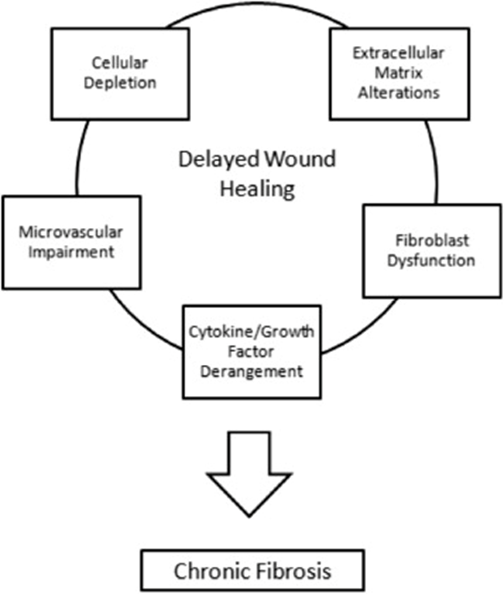
The Effects of Radiation
Radiation cause a progressive perivascular obliterative arteritis, poor O2 diffusion from capillary
Poor O2 tension at cellular level
Wound healing progressively worse over time
Beware operating on radiation damaged tissue
Adipose stem cell/fat grafting aids wound healing
Replacement of radiated tissue



Comments
Post a Comment